1st COVID-19 patient admitted to Alternate Care Facility

First patient admitted to Alternate Care Facility
The first patient was admitted to the Alternate Care Facility at Wisconsin State Fair Park seven days after it opened.
WEST ALLIS, Wis. - The first patient was admitted to the Alternate Care Facility at Wisconsin State Fair Park Wednesday, Oct. 21, the Wisconsin Department of Health Services' website shows, seven days after it opened.
“We are thankful to have this facility available to Wisconsinites and our hospitals, but also saddened that this is where Wisconsin is at today,” said Governor Tony Evers in a news release Wednesday afternoon. “Folks, please stay home. Help us protect our communities from this highly-contagious virus and avoid further strain on our hospitals."

COVID-19 alternate care facility at Wisconsin State Fair Park
DHS officials on Wednesday reported 4,205 new cases of COVID-19 bringing the cumulative number of cases to 182,687, also reporting that 1,681 people have now died due to COVID-19 complications -- an increase of 48 from Tuesday. The rise in deaths associated with the virus is a single-day record. Previously, the most deaths reported in a single day was 34 on Oct. 13.
The alternate care facility for COVID-19 patients opened at Wisconsin State Fair Park on Oct. 14, staffed with 50 doctors, nurses, pharmacists and other specialists. The facility, which was built in April, is able to accommodate as many as 530 patients.
The governor's news release Wednesday said patients at the facility who meet specific clinical criteria directly from hospitals' ERs will be given Remdesivir, and the facility's oxygen treatment capacity will be increased.
As of Wednesday, state health officials said Wisconsin continues to see high levels of COVID-19 hospitalizations, with some regions reporting over 90% utilization of ICU beds. The 7-day average of new cases reached nearly 3,500 for the first time since the pandemic began.

Signe Jorgenson
On Oct. 8, Sheboygan resident Signe Jorgenson learned firsthand just how overwhelmed the state's hospital system is.
"It was scary," said Jorgenson. "We didn't know what was going on, and the hospitals didn't really either."
Her 80-year-old father, Larry Jorgenson, wasn't infected with the virus, but he would spend 36 hours in search of immediate care because of it.

Larry Jorgenson
"He actually spent less time in a hospital bed than he spent looking for a hospital bed," said Signe Jorgenson.
Larry Jorgenson, who lives in an assisted living home in Wisconsin Rapids, fell and hit his head. He was taken to the only emergency room in the central Wisconsin town, where Signe says he was discharged too soon.
"When the nurses at his home went to wake him up, they couldn't wake him up," she said.
With no available beds at the hospital, he had just come from, Larry Jorgenson was taken to urgent care in Stevens Point, which wasn't equipped to handle his needs. A total of five ambulance rides later, he was finally admitted to a hospital in Wausau -- alone and scared. You see, not only had he suffered a head injury, he also has dementia.
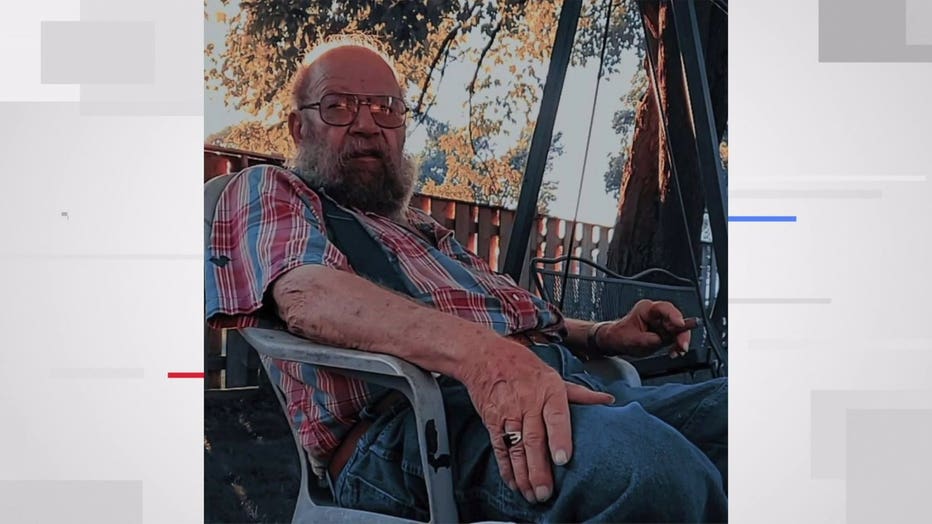
Larry Jorgenson
"He didn't understand what was happening, where he was going, why he was going," said Jorgenson.
With her father now back home and doing well, Signe wanted to share the traumatic ordeal as a warning to others, and a reminder that her father's situation could have been prevented.
"It doesn't matter if you have covid or not," she said. "If the hospitals are full and you have a heart attack, that's a problem. We need to do everything we can so that we aren't the next person who's riding around in five ambulances looking for a hospital bed."

Alternate care facility at Wisconsin State Fair Expo Center for treating COVID-19 patients
When the facility opened, officials said those admitted will already be on the road to recovery from the coronavirus, nearing discharge. They will have to meet a list of criteria that includes being between ages 18 and 70 with good vitals and a temperature of 100 degrees or lower.
The goal is to help take the pressure off of hospitals. Ultimately, the transfer of patients to the alternate care facility would allow hospitals to make more room for and devote more resources to COVID-19 and non-COVID-19 patients in need of urgent care.
"If we hear from health systems across the state, that we need to increase (beds) rapidly, we can go up to 75, 100 beds in a rapid amount of time," said Dr. Deb Standridge, CEO of the alternate care facility.
Patients who receive care at the alternate care facility will be there for approximately 3-6 days and will not be charged for their stay. They will be transported via ambulance to the facility by paramedics who have special training and PPE.
The facility does not accept walk-ins; patients must be referred by a hospital.

